BALTIMORE– For those striving to manage opioid use disorder, daily, in-person dosing (Directly Observed Therapy, or DOT) is the standard of care. While DOT secures high rates of adherence, it also presents major barriers to access and increased risks. But a new pilot study published in The Journal of Substance Abuse Treatment suggests that technology-enabled remote observation of methadone doses, using asynchronous video DOT, could allow opioid treatment programs to increase methadone adherence, reduce the barriers associated with in-person requirements, and help address the current behavioral health backlog.
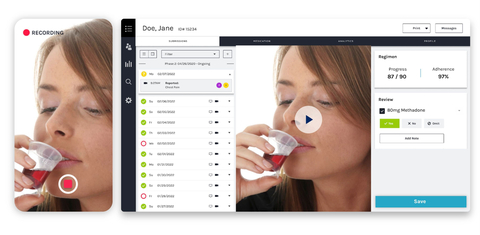
Conducted by The University of Washington School of Medicine, the study used emocha Health’s patient-facing mobile medication engagement app and provider-facing portal to provide daily video DOT for patients taking methadone. The pilot study was made possible when COVID-19 led to adjusted rules allowing patients to receive more frequent take-home doses to minimize in-person clinic visits. The study found that video observation of methadone take-home dosing is a practical and credible way to observe methadone dosing while reducing barriers that arise from requiring patients to come into a clinic. Among trial participants, 88% continued the trial for at least 60 days, and 61% of the pilot participants received increased take-home dosing privileges, which eliminated the need for additional in-person clinic visits.
“Our findings suggest it is feasible for counselors and patients to use this app, which provided confirmation of treatment while allowing them to not come to the clinic daily and to live their lives more fully,” said Dr. Judith Tsui, the study’s senior author and a professor of medicine at the University of Washington School of Medicine.
For the study, the clinical pilot program took place over five months at three opioid treatment programs in Washington State. Most patients had Medicaid insurance, and twenty-one percent were homeless. Pilot participants using the platform had a far higher number of days with an observed dose (on average 53.15) than matched controls (on average 16.64 days) who did not use the platform, suggesting that video DOT can increase assurance about methadone adherence.
“We think the technology can provide a middle ground, where doses can be observed and confirmed with less hassle and less potential exposure to diseases like COVID-19,” said Kevin Hallgren, the study’s lead author and a UW associate professor of psychiatry and behavioral sciences.
By demonstrating the feasibility of video technology in the remote observation of methadone treatment, this study suggests that video DOT is a viable service model for methadone dosing observation that will provide greater treatment flexibility for patients and healthcare professionals.
“Ensuring that every patient is able to take their medications as prescribed is our primary goal at emocha. This study clearly demonstrates that our technology can provide a more patient-centric approach to treatment without compromising the standard of care. The use of emocha resulted in more observed doses; regulators should act quickly to allow remote dosing in order to increase access to methadone treatment as opioid overdose deaths continue to skyrocket,” said emocha CEO, Sebastian Seiguer.
Change can come quickly — in a span of eight years since 2014, emocha has brought remote observation capabilities to more than 400 public health departments across the country who use emocha for infectious disease DOT, as well as Medicaid health plans using emocha for asthma, diabetes, and hypertension. Video DOT is now considered the standard of care for tuberculosis control programs in the United States.
emocha Health’s technology has been studied in multiple clinical trials led by The University of Washington School of Medicine. In 2016, a study involved video DOT for Hepatitis C (HCV) medication adherence among injection drug users and in 2018, a study involved technology that supports patient-centric care for opioid use disorder. emocha’s platform and video DOT has now been shown effective at remotely supporting adherence across several chronic and infectious conditions, such as asthma, hepatitis C, tuberculosis, solid organ transplants, and sickle cell disease.