LA JOLLA, Calif.– As people live longer than ever before, the incidence of aging-related, chronic diseases is on the rise, severely impacting quality of life and placing an unprecedented financial and care burden on overwhelmed families, government agencies and healthcare providers.
To help address this growing challenge, scientists at Scripps Research and its nonprofit drug development arm, the Calibr-Skaggs Institute for Innovative Medicines, are advancing novel regenerative medicines capable of repairing tissues damaged by age-related disease. In contrast to cell therapies, these first-in-class small molecule drugs—several of which are already in preclinical and phase 1 clinical trials—act on endogenous stem cells in the body to control their fate. They are being developed to treat osteoarthritis, inflammatory bowel disease, lung diseases, heart failure, macular degeneration and more.
“Current therapies for these chronic conditions slow disease progression or treat the symptoms, but don’t fully stop or reverse the resulting damage,” says Peter Schultz, PhD, President and CEO of Scripps Research. “In contrast, the regenerative medicine pipeline at Scripps Research represents a new frontier in healthy aging, with disease-modifying therapies that repair damaged tissues and thereby restore function in patients.”
Scripps Research and Calibr-Skaggs’ programs in development include:
- Lung: Restoring lung tissue to treat pulmonary disease – Respiratory disease is the third leading killer globally. The ability to repair damage to the lung by stimulating growth of stem cells in the lower airway, called type 2 alveolar epithelial cells (AEC2s), could reverse loss of lung function caused by lung disease. Scripps Research and Calibr-Skaggs have developed a once-weekly, inhaled drug, CMR316, that promotes AEC2 stem cell expansion and the formation of new lung cells responsible for gas exchange. CMR316 promotes lung repair in several animal models of lung damage, including emphysema, chronic obstructive pulmonary disease (COPD) and IPF. CMR316 is currently undergoing a phase 1 clinical trial in healthy volunteers and IPF patients.
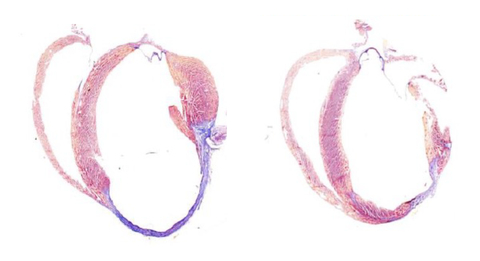
- Heart: Regenerating cardiac tissue after a heart attack – Heart disease is the leading cause of death globally. Cardiomyocytes—the muscle cells of the heart—are unable to regenerate tissue after a heart attack, often resulting in progressive disease and scarring. Scripps Research and Calibr-Skaggs are developing a small molecule drug (CMV852) that activates a regenerative pathway through YES-associated protein 1 (YAP) to stimulate the growth of new heart cells. This drug is injected precisely at the site of the damage in the heart, and it has already shown the ability to induce new functional cardiac tissue and significantly improve heart function in mice and pigs after a heart attack. CMV852 is expected to initiate investigational new drug (IND)-enabling studies in 2025.
- Cartilage: Repairing cartilage to address osteoarthritis (OA) – OA, a disease involving degeneration of joint cartilage and chronic pain, affects more than 30 million individuals in the U.S. Calibr-Skaggs is developing the small molecule, KA34, to promote robust regeneration of lost cartilage in animal models of OA, resulting in new functional joint tissue and decreased pain. KA34 has undergone extensive preclinical testing and shown good safety in a phase 1b human trial. Calibr-Skaggs scientists are currently developing extended-release formulations of KA34 to enable the drug to stimulate cartilage growth over longer periods (3 to 6 months), which will reduce the frequency of injections and patient burden.
- Eye: Repairing the retina in macular degeneration – Age-related macular degeneration (AMD) is the most common form of vision loss associated with age, affecting nearly 13% of people 40 and older. AMD is associated with the loss of retinal pigment epithelial cells (RPEs) due to age and oxidative damage. Scientists have identified several small molecule drugs that selectively expand RPEs to regenerate a functional RPE layer, which are being evaluated in laboratory and animal studies to determine which of several mechanisms would be most amenable as an AMD therapy. If successful, the envisioned therapy would be a one-time injection of a long-acting drug to replenish the RPE layer in people with early-stage AMD.
- Intestine: Restoring the intestinal barrier for inflammatory bowel disease (IBD) – IBD, including Crohn’s and ulcerative colitis, results from auto-inflammatory destruction of the gastrointestinal tract. Calibr-Skaggs has developed a long-acting, chemically modified GLP-2 mimetic that robustly promotes healing in the gut and restores the mucosal barrier function. This agent has undergone a successful phase 1 clinical trial in humans, demonstrating safety, a best-in-class half-life and upregulation of a key biomarker of intestinal repair. Calibr-Skaggs or its partner will be conducting a phase 2 study to evaluate the efficacy of the clinical candidate in patients with IBD and IBD-related disorders.
Michael Bollong, PhD, associate chemistry professor and the Early Career Endowed Roon Chair for Cardiovascular Research at Scripps Research, who led the discovery of several of the regenerative programs, along with Schultz, who is also a professor of Chemistry, notes that the Scripps Research/Calibr-Skaggs team’s approach focuses on the development of small molecule drugs designed to be more accessible and easily administered than stem cell therapies.
With conventional cell-based therapies stalled by complexity, poor efficacy and high costs, these small molecules provide a path forward for more effective regenerative medicines. “Our ultimate goal,” says Bollong, “is to expand to other organs to repair disease-related injury or even to rejuvenate healthy tissues as we age.”
Schultz adds, “If we are able to show these therapies work in a disease setting, the next question will be to ask if they reverse age-related damage in otherwise healthy aging adults.”