MANHASSET, N.Y.– A hallmark of fatal SARS-CoV-2 infection (COVID-19) is cytokine storm – an increase of inflammatory proteins within the body – that can lead to respiratory distress and organ failure. A new study published today in the Journal of Internal Medicine (JIM) by researchers at The Feinstein Institutes for Medical Research and the Karolinska Institutet discuss the relationship between COVID-19, the vagus nerve, the body’s inflammatory reflex and the therapeutic potentials to treat the disease and long-COVID.
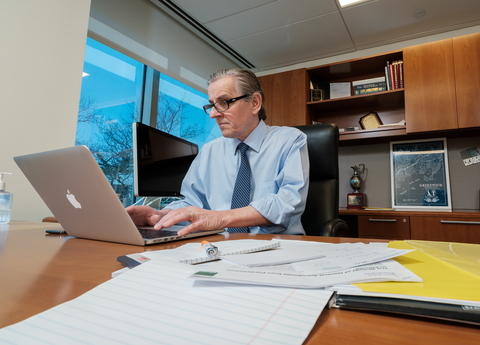
The paper, titled “Vagus Nerve SARS-CoV-2 Infection and Inflammatory Reflex Dysfunction: Is there a causal Relationship?” written by Kevin J. Tracey, MD, president and CEO of the Feinstein Institutes and Ulf Andersson, PhD, professor emeritus in the Department of Women’s and Children’s Health at the Karolinska Institutet, looks at the current research and evidence that impairment of the body’s vagus nerve inflammatory reflex may contribute to the overproduction of cytokines and hyperinflammatory progression of COVID-19.
“The discovery that SARS-CoV-2 can infect the vagus nerve introduces new questions for researchers studying both COVID-19 and post-COVID-19 syndrome,” said Dr. Tracey, who is the Karches Family Distinguished Chair in Medical Research. “This paper raises foundational questions for future basic and clinical investigations, aiming to study innovative therapies for addressing the disease and its long-term complications.”
Originating in the brain and extending to the body’s organs, the vagus nerve helps communicate and maintain how the body functions, including heart rate, breathing and immune response, and the release of inflammatory proteins like high mobility group box 1 protein (HMGB1). This neural communication pathway, which is meant to sustain the body’s natural state or homeostasis, was previously discovered by Dr. Tracey, which he termed the “inflammatory reflex.” If the vagus nerve and the inflammatory reflex are compromised, too much or too little inflammatory proteins are released in the body, causing diseases like rheumatoid arthritis, Crohn’s disease or, as evidence shows, respiratory impairment and hyperinflammation in people with COVID-19.
Drs. Tracey and Andersson cite evidence in the current paper that shows SARS-CoV-2 infection within the vagus nerve at the acute stage of the disease may hamper its inflammatory reflex and proper functioning. They outline existing research looking at the interplay between two molecules, HMGB1 and acetylcholine, and the role of regulating inflammation. They also discussed potential therapies, particularly to reduce the progression of COVID-19 in infected patients as well as long COVID-19 treatment options. Famotidine, a histamine 2 receptor-antagonist, has been shown to attenuate the clinical course of COVID-19 and may be an inexpensive and safe way to treat the disease. However, future study is needed. Additionally, the role of electronic vagus nerve stimulation (VNS) was discussed in the paper. VNS can be performed using surgically implanted cervical vagus nerve electrodes or non-invasive transcutaneous electrical vagal stimulation and help “reset” the vagus nerve to regulate better and prevent the increase of inflammatory proteins.
“Studying the connection between COVID-19 and the vagus nerve is an important research avenue that needs further study,” said Dr. Andersson. “We need to understand better the underlying molecular mechanisms of the disease to develop new clinical treatments that can aid individuals infected with SARS-CoV-2 and in their recovery.”
Recent data demonstrates that the vagus nerve is infected and inflamed during severe COVID-19. That understanding raises many questions and potential pathways of research to develop new ways of preventing potentially fatal disease progression and long-lasting effects of COVID-19.
The Feinstein Institutes for Medical Research is the global scientific home of bioelectronic medicine, which combines molecular medicine, neuroscience, and biomedical engineering. At the Feinstein Institutes, medical researchers use modern technology to develop new device-based therapies to treat disease and injury.
Built on years of research in molecular mechanisms of disease and the link between the nervous and immune systems, our researchers discover neural targets that can be activated or inhibited with neuromodulation devices, like vagus nerve implants, to control the body’s immune response and inflammation. If inflammation is successfully controlled, diseases – such as arthritis, pulmonary hypertension, Crohn’s disease, inflammatory bowel diseases, diabetes, cancer and autoimmune diseases – can be treated more effectively.
Beyond inflammation, using novel brain-computer interfaces, Feinstein Institutes researchers developed techniques to bypass injuries of the nervous system so that people living with paralysis can regain sensation and use their limbs. By producing bioelectronic medicine knowledge, disease and injury, could one day be treated with our own nerves without costly and potentially harmful pharmaceuticals.